Increase your chances of surviving breast cancer by knowing risk factors and following screening recommendations.
Few diseases have benefited from increased awareness in the past few decades in the way that breast cancer has. Breast cancer is the most common cancer diagnosed in women in the United States and accounts for about 30 percent of all new cancer diagnoses in women each year. The American Cancer Society estimates that about 42,250 women die annually from breast cancer.
While the numbers are sobering, we should also note and celebrate the rise in breast cancer survivorship rates. This is due to a combination of increased awareness, improved screening, and better treatments. For this post, we’ll highlight some risk factors for cancer and discuss current screening approaches.
Breast cancer risk factors
Risk factors for breast cancer are varied and include some that cannot be changed, like rising age, certain inherited genetic mutations like BRCA, family history of breast cancer, or prior history of radiation to the chest. A longer period of exposure to hormones between menarche (onset of menstruation) and menopause, or taking external hormone therapy can also increase the risk. For the same reason, becoming pregnant, especially earlier in life, can protect against cancer risk as can breastfeeding. Alcohol use, low levels of physical activity, and having excess weight post-menopause are all modifiable risk factors. Having dense breast tissues is also a risk factor for developing breast cancer. Fortunately, while breast density cannot be changed, mammograms now report this finding, thereby increasing awareness.
Screening for breast cancer
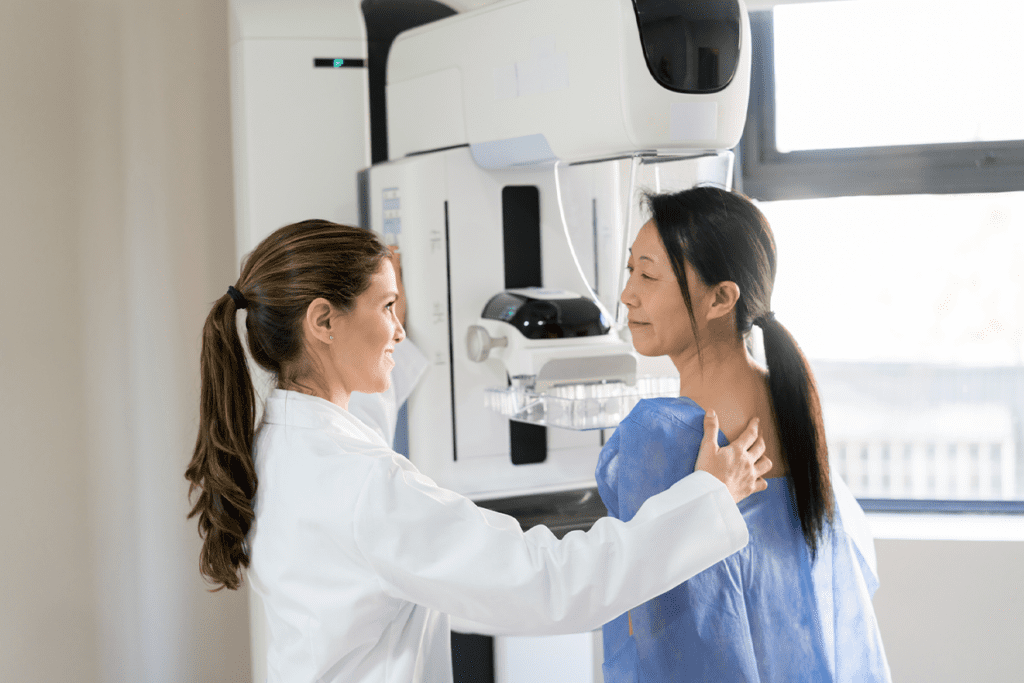
Screening for breast cancer is done mainly through mammograms, which refer to X-rays of the breast. In addition to noting the presence of potential cancer, mammograms also comment on density of the breast. This can be confusing to patients and is worth clarifying. As noted earlier, dense breast tissues can increase risk for breast cancer and these mammogram reports serve as a way to inform patients of that risk. Additionally, dense breasts also make it harder to spot cancers. Breast self-exams by patients are popular and are a way for women to note something abnormal in their breast. However, this has not been shown to reduce risk of dying from breast cancer and therefore cannot replace a mammogram when recommended.
Magnetic Resonance Imaging (MRI) can also be used but is often reserved for women at higher risk. That’s because in someone at average risk, they can appear abnormal even when no disease exists.
Screening timetable
Finally, it’s worth discussing when screening needs to begin. The United States preventive services task force (USPSTF) had previously recommended screening starting at age 50 for most patients and is currently reviewing its guidelines. While UPSTF has yet to issue its final recommendation, it is widely expected to move that forward to age 40 for women at average risk. In women at high risk due to family history, screening often commences earlier – typically ten years before the earliest age at which a family member was diagnosed with breast cancer.
To summarize, breast cancer is a scary diagnosis that as many as one in eight women will face in their lifetime. Fortunately, you can address this risk through active screening. So if you have not already discussed this with your healthcare provider, be sure to bring it up to learn more of your own risk!
Disclaimer: This blog content and linked materials are not intended as individual medical advice, diagnosis or treatment, and should not be considered as such. Any readers with medical concerns should contact a licensed healthcare provider. This blog is provided for informational purposes only.
