Injectable PrEP is a game changer in protecting people against HIV infection. One challenge is educating more providers about this important tool so they can offer it to patients.
Pre-exposure Prophylaxis (PrEP) against Human Immunodeficiency Virus (HIV) was first approved in 2012. At the time, the only approved option was an oral pill under the brand name Truvada. Since then, there have been several advances in PrEP. In 2019, a second oral medication under the brand name Descovy was approved and it offered a better safety profile for patients with kidney disease. However, in 2021, the Food and Drug Administration (FDA) approved Cabotegravir as the first injectable treatment for PrEP.
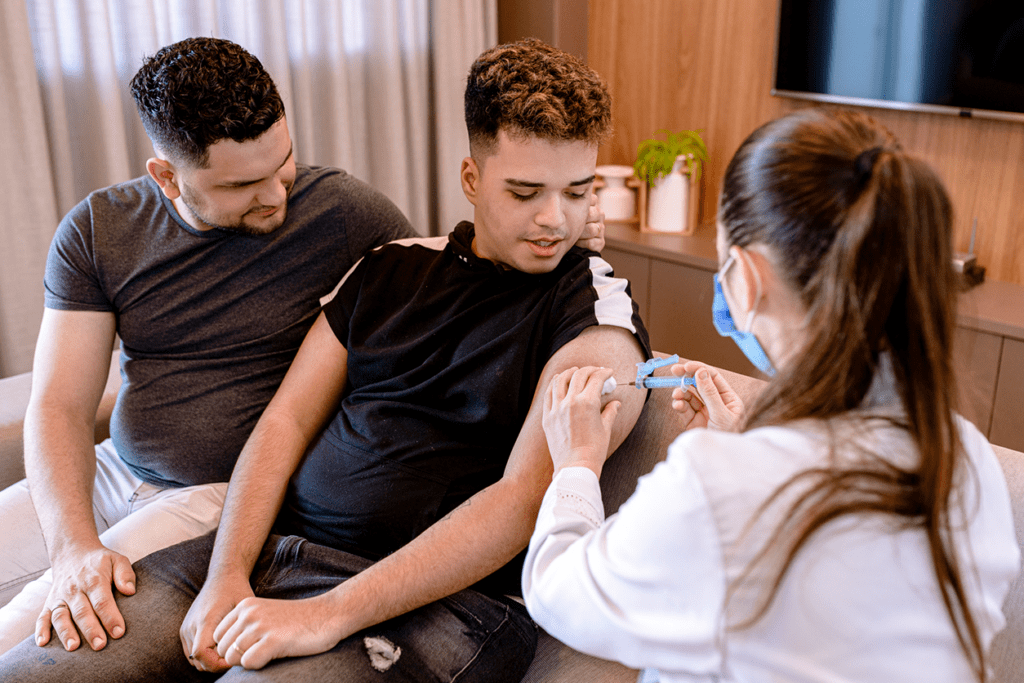
What makes Cabotegravir truly game changing is that it can be administered once every two months. This makes it much easier for patients who struggle with remembering to take a daily oral medication. This is particularly important as a lot of patients at risk for HIV are younger and not accustomed to managing daily medications. Another obvious advantage is that patients do not need to stock any medication at home. This benefits patients who may not feel comfortable disclosing medication use with others in their household for various reasons, including threat of violence.
Injectable PrEP 101
The first question my patients ask about injectable PrEP is how its effectiveness compares to oral PrEP. Fortunately, data is very encouraging on that front. Patients who used injectable Cabotegravir have a 69% lower risk of getting HIV when compared to those taking oral Truvada.
Also, injectable PrEP is easy to administer during a clinic visit. The first two doses are delivered a month apart but subsequent doses are delivered once every other month. As with oral PrEP, it is important to get baseline labs and regular screening labs once the injections have started. It does not appear to increase the risk of kidney issues in a manner similar to Truvada but it does carry additional side effects associated with injections, such as a local reaction or infection. As with all PrEP, it only protects you from getting HIV. Adopting other measures around safe sex is important to lower the risk of other sexually transmitted infections like syphilis, gonorrhea, or chlamydia.
PrEP hurdles
Injectable PrEP is not without its potential challenges. For one, many people simply do not like getting an injection on a regular basis. Also, it obviously requires regular office visits every few months, which can also be a challenge for some patients. But perhaps the most pressing challenge is that not all providers know enough about injectable PrEP to offer it to their patients. This makes access challenging even when a patient feels ready to start injectable PrEP.
At Primary.Health, we are focused on reducing barriers to seeking PrEP and believe that designing workflows that support patients is key to increasing access to PrEP.
Disclaimer: This blog content and linked materials are not intended as individual medical advice, diagnosis or treatment, and should not be considered as such. Any readers with medical concerns should contact a licensed healthcare provider. This blog is provided for informational purposes only.
